In collaboration with Charter Senior Living
The onset of COVID-19 has certainly caused much unrest and concern around the care of our loved ones. This is especially true for older generations residing in senior living communities. Nevertheless, the past few months have offered significant learning opportunities on how to best respond to the spread of COVID-19. If you’re in need of solutions to keep your elder residents and patients safe, there are several best practices you can follow. ERDMAN, in collaboration with Charter Senior Living, has identified four ways to retrofit senior living communities for infection control:
Adjust or Renovate Your Facility to Manage and Support Isolation Scenarios
Lobbies and reception areas can be transformed into front-line zones where visitors undergo various screening measures to reduce the potential for transmitting the virus. This can be achieved by implementing new technologies and systems that are proactive in stopping the spread of diseases. Examples include:
- Sanitizer Dispenser Mats: This technology sanitizes shoes upon entry. As people step on the mat, sanitizer is applied to people’s shoes, killing germs trapped in the crevices. In turn, sanitizer dispenser mats help reduce the chance of cross contamination.
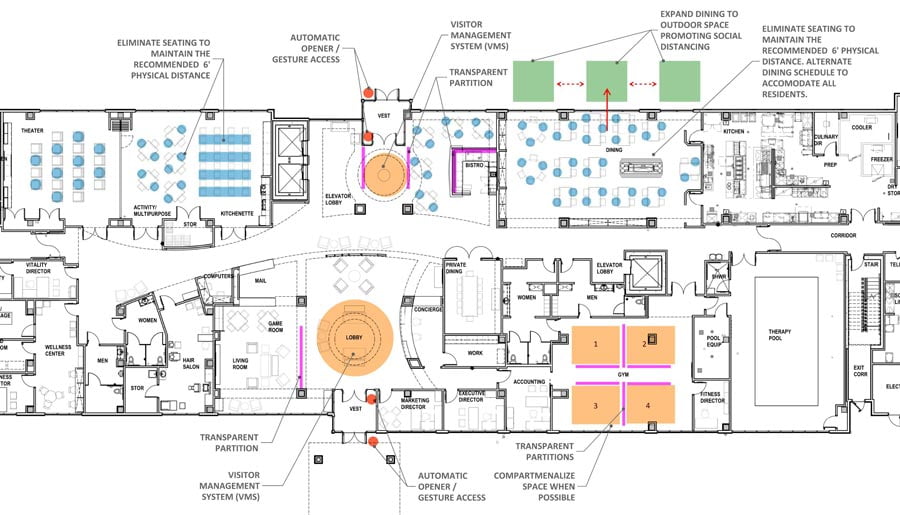
- Small, self-contained neighborhoods: “Compartmentalizing large spaces into smaller areas can be an effective design strategy. As this tactic can minimize the number of residents in a space, it reduces the source transmission of germs,” explains Maura Feaheny, Vice President of Development & Strategy with Charter Senior Living. Areas that can be compartmentalized include living spaces, staff work areas, dining, and amenities. It should also be noted that such areas may need to be closed off if quarantining is required for the safety of residents and staff. Thus, the flexibility and agility of the contained areas are key. For example, as seen in the floor plan below, tables and chairs can be rearranged to maintain a safe distance and limit the number of people that gather in a place at one time. Plexiglass partitions can also be set up on tables between diners to minimize exposure to other residents.
Encouraging Social Distancing and Creating Self-Contained Neighborhoods
In assessing ERDMAN’s GenCare Lifestyle at Point Ruston, a senior living community offering assisted and independent living, various areas presented opportunities to mitigate the spread of COVID-19. Rearranging furniture, using partitions, and eliminating some seating help create self-contained areas and enable social distancing, allowing GenCare’s various amenities to still be enjoyed by residents.
- Visitor Management System: Cloud-based visitor management systems like Fidentity, Veris, and Accushield provide touchless check-in experiences. Such systems are valuable in that they limit the number of surfaces that visitors touch, which in turn can minimize the transfer of COVID-19. These systems leverage personal-protective-equipment (PPE) scanning, facial recognition, mask detection, and temperature scan sensors using artificial intelligence. A PPE station can also be added as part of a building’s entry where visitors sanitize their hands, wear gloves, and put on clean masks to further mitigate the spread of infections.
What Does a Visitor Management System Look to Support in Isolation Scenarios?

PPE SCANNING
Allows the scanning of people to ensure they are following safety protocols

FACIAL RECOGNITION
Verifies who is entering the building and allows check-in without touching a kiosk

TOUCHLESS CHECK-IN
Allows visitors and employees to complete a touchless check-in process using their mobile devices and scanning QR codes

TEMPERATURE SCREENING
Monitors the temperature of visitors and employees upon entry of the building, providing an extra safety measure
Reduce Potential for High-Traffic Contact Transmission
- Low- and no-touch door hardware and switches: Low- and no-touch building features help control the spread of infection as they minimize the amount of contact people can have with different surfaces. For example, Wi-Fi switches can be controlled via an app, physical touch, or voice control through a smart speaker such as Amazon Echo or Google Home. Sound or motion activated switches can also be utilized. However, it should be noted that most energy codes currently require the physical operation of a light switch.

- Smart materials: Different materials and technology exist that can inhibit the growth of damaging microorganisms. For example, Microban® uses silver and copper ion antimicrobial technology that can be applied in solid surfaces, bed rails, door hardware, grab bars, light switches, textile base materials, and porcelain tile. When microbes meet a surface, Microban® penetrates the cell wall of microorganisms and disrupts cell growth and reproduction, making it unable to function.1 This works to eliminate microbial growth on surfaces with no impact on aesthetics. There are also technologies that utilize light to kill bacteria. ACTIVE® ceramic is one such example. It employs an oxidation process introduced by photocatalysis to destroy bacteria on surfaces.
Adding handwashing stations to your facility could make a big impact on keeping residents and staff healthy as handwashing removes pathogens and essentially can inactivate the virus.
- Handwashing stations: An important infection-control strategy is hand hygiene. However, current senior living buildings likely lack access to handwashing stations outside of tenant living space since hand hygiene was not critical prior to the onset of COVID-19. If adding handwashing stations to your facility is possible, it could make a big impact on keeping residents and staff healthy as handwashing removes pathogens and essentially can inactivate the virus.2 To do so, there are key considerations to keep in mind. For example, handwashing sinks and faucets should be selected that avoid splashing. They should also not be near waste outlets to prevent water contamination. Additionally, sinks should have a depth that allows for washing and rinsing of the forearms up to the elbow. Great manufacturers to consider for such handwashing stations are Willoughby and Whitehall.
- Disinfection protocols: High-touch surfaces including tables, doorknobs, light switches, countertops, handles, phones, keyboards, toilets, faucets, and sinks should be identified as priority disinfection areas. Disinfection protocols recommended by the CDC are:
- Clean surfaces using soap and water, then use disinfectant
- Practice routine cleaning of frequently touched surfaces
- More frequent cleaning and disinfection may be required based on level of use
Understand that HVAC Systems are Part of the Solution, Not Part of the Problem
As the pandemic continues, more information is becoming available on how it can spread and be airborne. For example, as explained by ASHRAE Epidemic Taskforce Chair and Penn State University Professor William Bahnfleth, the main way a building’s air conditioning can contribute to the spread of the virus is by creating strong air currents that move droplets carrying COVID-19.3 In turn, ventilation systems within senior living communities deserve much attention. To address the issue, senior living operators should be asking certain questions: Are ventilation systems optimized to mitigate the spread of the virus? What are the options to improve our ventilation systems to keep our community safe and healthy?
To address such questions, ASHRAE recently published its Position Document on Infection Aerosols. It explains that facilities of all types should follow, at a minimum, the latest published standards and guidelines, as well as good engineering practices.4 “In terms of senior living communities, most are required to follow ASHRAE Standard 170 for their minimum level of ventilation. Examples include minimum levels of air filtration, as well as changes in outdoor air and total ventilation air provided to various room types,” explains Michael Meteyer, Engineering Manager for ERDMAN and member of ASHRAE Standard 170.
Considering such guidelines, the first step is making sure ventilation systems are meeting requirements that were in place at the time they were installed. Next, it is important to compare current ventilation levels to the latest ASHRAE Standard 170 requirements. As a third step, a risk assessment, combined with a cost-benefit analysis, can be used to evaluate options to correct deficiencies and exceed minimum standards. In doing so, there are four key strategies to consider:
Did You Know?
ASHRAE stands for the American Society of Heating, Refrigerating and Air-Conditioning Engineers. As a professional organization, it focuses on building systems, energy efficiency, indoor air quality, refrigeration, and sustainability. It performs research, establishes standards, offers ongoing education, and more to shape the built environment.5
Also, the most common filter rating is the Minimum Efficiency Reporting Value (MERV). Filters are rated between MERV 1 to MERV 16. The higher the MERV rating, the higher the effectiveness. Specifically, the rating represents the filter efficiency by means of measuring the fraction of particles removed from the air under standard conditions.
Another filtration rating system that is commonly used is High Efficiency Particulate Air (HEPA). HEPA filters are more efficient than most MERV filters. For example, in the context of COVID-19, the virus is approximately 0.12 µm in diameter and is typically attached to other particles. HEPA filters, and MERV 14 or higher filters, are very effective at capturing the size of such particles as the filters can prevent the particles from being recirculated through ventilation systems. However, many systems are not capable of being retrofitted with the filters because of the additional fan horsepower required and the additional physical space needed for their depth and the mounting frame.
- Filtration (air cleaning): Increasing the level of filtration in ventilation systems is a proven method to reduce particle contaminants. “It is also likely the most cost-effective option for improving a facility’s air quality,” Meteyer says based on his 30 years of experience in designing and commissioning healthcare facility systems. For example, the code requires that air filters are rated at least a MERV 7. However, a MERV 7 is less than 20 percent effective at capturing the particle size of +/- 0.3 microns, which is capable of penetrating the deepest level of our lungs. Increasing the filters to a MERV 13 will improve the effectiveness to over 50 percent, and HEPA rated filters are 99 percent effective for this size of particle. However, many systems were not designed with this higher level of filtration in mind. This is important to note as higher rated filters require more fan horsepower and are typically larger in size. Prior to retrofitting the systems, they will need to be evaluated to determine the horsepower capacity and the additional physical space needed to improve the level of filtration.
If your facility does not have the ability to install MERV 13+ or HEPA filters, maintenance staff should take precautions using PPE to carefully bag and dispose of the filters as they could be holding virus particles. It is also recommended to spray the filters with hair spray or paint prior to removal.
Increasing the filters to a MERV 13 will improve filtration effectiveness to over 50 percent, and HEPA rated filters are 99 percent effective.
- Outside air (dilution): Increasing the outside air supplied to the indoors will dilute contaminants in a space. This is important to consider as the concentration of viable virus particles is a factor in transmitting COVID-19. In normal circumstances, certain building areas are required to have a minimum amount of outside air (i.e. fresh air). That said, you may be asking yourself: Are my building systems meeting the minimum requirement? And is there a cost-effective option to increase the amount of fresh air beyond the minimum? In answering these questions, you’ll want to consider how various types of systems limit the amount of outside air used to cool a space. In addition, more outside air typically requires more energy, which can impact costs.
- Air movement (pressurization): Components of HVAC systems at times can be used to generate relative air pressure differences that will produce an airflow direction. For example, creating a positive pressure is used to protect or limit contaminants from migrating into a space. In contrast, a negative pressure directs airflow into a space that can prevent migration out of a space. “This strategy will have limited opportunities in most existing senior living communities. However, one solution to consider is when a building wing is going to be used as cohort for positive, or potentially positive, COVID-19 residents. This area could then potentially have a negative air pressure relative to the other community areas. In turn, it could help reduce the potential for contaminating other parts of the building,” says Feaheny.
- Air disinfection: The last strategy is considering air disinfection. Some options are focused on cleaning the air in the space itself, while others pertain to HVAC systems. Technologies for air disinfection include ultraviolet germicidal irradiation (UVGI), bipolar ionization, and photocatalytic oxidation. Some of the options are permanently located and others are portable. Many of these newer technologies do not necessarily have industry-wide consensus on their effectiveness. Generating potentially harmful by-products and understanding how to safely use such technologies are concerns that still need to be fully vetted.
Integrate Improved Video and Telecommunications into Senior Living Communities
The World Health Organization identified physical distancing as an essential precaution to reduce the chances of spreading COVID-19. However, in an effort to flatten the curve, physical distancing resulted in social isolation and loneliness, especially for seniors.6 For example, a report by The National Academies indicated significantly higher rates of heart disease, stroke, and a 50 percent increase in the risk of dementia among isolated, lonely seniors. The report also noted increases in depression and anxiety.7 To counter the health issues stemming from isolation and loneliness, it is imperative to foster mental health through design while social distancing. For example, virtual communication and relevant training of new technology can keep seniors connected with loved ones. Virtual reality can even be utilized to enhance seniors’ quality of life while battling isolation as they share 360-degree experiences in their own communities such as mountain climbing, hot air balloon rides, and more.

As it is important to keep seniors connected with family, it is also critical to keep them connected with their medical providers. Since the start of the pandemic, there has been a significant increase in the use of telehealth. The challenge for senior living providers now is caring for residents while enforcing social distancing and other clinical strategies to reduce the risk of COVID-19 transmission. To achieve this, providers can create dedicated rooms for telehealth sessions or provide carts with video conferencing technology that can be moved around throughout a senior living community.
ERDMAN Takeaway
There is no doubt that the world could not have anticipated the impact COVID-19 has had on our lives. Nevertheless, we have found that there are multiple ways to adapt facilities to keep senior living communities and their staff safe. If done properly, not only will you be supporting the physical health of your residents, but also their mental health. Additionally, retrofitting facilities will improve your buildings’ flexibility and resilience in dealing with infectious disease threats. If you need additional guidance on how your building can better support your residents and staff, ERDMAN would love to connect with you. Our decades of experience and insights into the industry can certainly help guide you as we all persevere through COVID-19 and design future senior living communities.
For more information, please contact us.

- FREQUENTLY ASKED QUESTIONS. (n.d.). Retrieved from https://www.microban.com/antimicrobial-solutions/resources-microban-antimicrobial-solutions/antimicrobial-definition-and-frequently-asked-questions
- “Hand Hygiene Recommendations.” (2020, May 17). Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/hcp/hand-hygiene.html#references
- Rodriguez, A. (2020, July 15). Most air conditioning systems don’t protect against the coronavirus. In some cases, they can actually facilitate spread. Retrieved from https://www.usatoday.com/story/news/health/2020/07/15/covid-air-conditioning-could-facilitate-coronavirus-airborne-spread/5429919002/
- “ASHRAE Position Document on Infectious Aerosols.” (2020, April 14). Retrieved from https://www.ashrae.org/file%20library/about/position%20documents/pd_infectiousaerosols_2020.pdf
- “About ASHRAE.” (n.d.). Retrieved from https://www.ashrae.org/about
- Torres, E. (2020, April 8). “Experts urge caution on possible ‘flattening’ of coronavirus cases: ‘Can’t say we’re out of the waters and safe’.” Retrieved from https://abcnews.go.com/Health/experts-urge-caution-flattening-coronavirus-cases-waters-safe/story?id=70018810
- National Academies of Sciences, Engineering, and Medicine. 2020. “Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System.” Washington, DC: The National Academies Press. https://doi.org/10.17226/25663