Loneliness and social isolation are prevalent and growing challenges in society. The pandemic has drawn attention to both issues, as well as efforts to mitigate their impact. Though often used synonymously, they’re not the same.
Social isolation is an objective measure of how much contact an individual has with others. In contrast, loneliness is a subjective measure of a person’s isolation. For example, an individual with limited social contact may not be lonely, while a person with significant social contact might be lonely. Distinguishing between the two is key. For example:
Social isolation should be approached as a physical distancing challenge. Solutions can involve safe proximity to family and friends, engagement in small groups of fewer than 10 people, as well as digital connectivity via social media and online chat technology.
Loneliness is more challenging. It should be approached as a clinical problem. Solutions could require a wide range of diagnostic and therapeutic resources to help mitigate its impact on people’s physical and emotional health.
Both social isolation and loneliness require thoughtful consideration. The lion’s share of attention during the pandemic has been given to social isolation as a byproduct of social distancing and lockdown policies. This has eased as vaccines have become available and restrictions on social gathering have been relaxed, but it remains to be seen whether the negative impact of social isolation has declined.
Loneliness, on the other hand, is more complicated. This is especially so for the senior population. Left unattended, it will have severe consequences for our older generations and healthcare systems, given that the senior population is increasing. According to the U.S. Census Bureau, our 65-and-older population has grown steadily for 70 years. Today, the nation’s 54 million seniors compose 16.9 percent of the U.S. population. This group is expected to reach 20.6 percent by 2030. No other age group is growing as fast as seniors.
A Snapshot of the Senior Population in the U.S.
- The nation’s 65-and-older population has grown steadily for 70 years.
- Today, 54 million seniors compose 16.9 percent of the U.S. population. This group is expected to reach 20.6 percent by 2030. No other age group is growing as fast as seniors.
- The 65-and-older population grew by 34.2 percent, which represents over 13.7 million people, during the past decade. By contrast, the nation’s under-18 population declined by 1.5 percent.
- The 80-plus population is projected to increase 79 percent by 2030.
- In 2010, the dependency ratio for the nation was 49. This means that for every 100 working-age people, there were 49 dependent-age people. By 2019, this dependency ratio increased to 53.7, which is driven by the growing 65-and-older population.

Considering such growth, the senior population plays a significant and growing role in our economy. This is especially true in healthcare. For example:
As we recognize such observations, it is also important to note that the senior market in the U.S. is not homogenous. According to ERDMAN’s tapestry analysis of the senior population, the group can be segmented into eight cohorts, three of which are distinctly described below. This segmentation not only considers age, but also the senior population’s lifestyle and purchasing habits. Segmentation can also expose populations at risk for loneliness based on social determinants of health, such as economic stability and access to transportation, healthy food options and healthcare, as well as community engagement.
Three Examples of Diversity Within the Senior Market
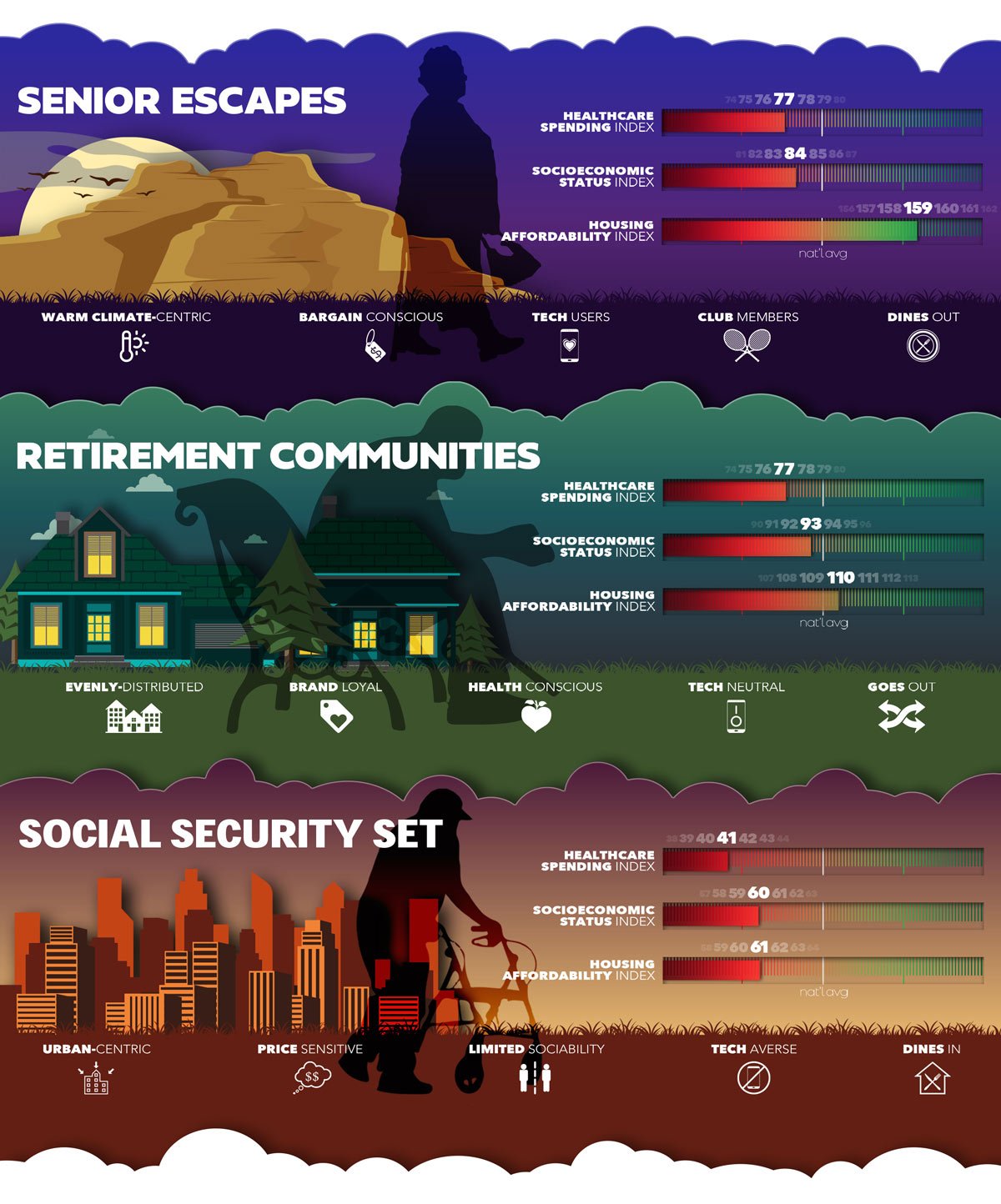
Although we have noticed that all seniors worry about health and wellbeing, and engage with health systems frequently, their buying patterns, social interactions, and attitudes vary. Differences based on social determinants, including social isolation, play a huge role in their health status. Consider the following:
- Nearly 20 percent of older adults report feeling lonely frequently, according to the 2019 National Social Life Health and Aging Project study.
- A January 2020 study by Cigna found that 50 percent of seniors experienced loneliness prior to the pandemic.
- An AARP study of adults, age 45 and older, found that among respondents who rated their health as “excellent,” only 25 percent were likely to be lonely, compared to 55 percent of those who rated their health as “poor.”

In the medical world, loneliness is not designated as a diagnosis. Specifically, it is not explicitly included in DSM-5, the official diagnostic manual for mental health disorders. Yet, clinical research has shown a significant correlation between senior loneliness and certain illnesses. Such health concerns include dementia, depression, anxiety, self-harm, heart disease, and substance abuse. According to the Foundation for Art and Healing:
Clinical research has shown a significant correlation between senior loneliness and certain illnesses.
- Health risks associated with loneliness and social isolation are comparable to the dangers of smoking and obesity, increasing mortality risk by up to 30 percent. Feeling alone also increases the risk of death by 26 percent, while social isolation and living alone increases mortality risk by 29 percent and 32 percent respectively.
- Loneliness has negative effects on mental health, anxiety, mood disorders, and physical health. It also can lead to worsening depression, cognitive decline, and higher rates of cardiovascular impairment, chronic pain, and fatigue.
- Older adults seem to be particularly at risk, marked by growing incidence of depression, substance abuse, and suicide.
Responding to Loneliness in the Senior Population: The Four Imperatives
Programs that explicitly address loneliness in the senior population are needed. A framework that offers a strategy to address loneliness in the senior population should include:
1. SCREENING IN PRIMARY CARE
According to the National Academy of Sciences, Engineering & Medicine, screening for loneliness is inadequate and often overlooked. While there is growing recognition that social determinants of health (i.e. food insecurity, safe housing, etc.) contribute to poor outcomes and higher health costs, loneliness has not been diagnosed specifically. Rather, it has been treated as social isolation, thus failing to detect and mitigate its clinical complications and associated costs.
Ongoing screening for symptoms of loneliness in primary care settings is foundational to treat loneliness among seniors. To do so, consider these commonly used screening tools:
- Campaign to End Loneliness Measurement tool
- De-Jong Giervald 6-Item Loneliness Scale
- UCLA 3-Item Loneliness Scale
- AARP’s Connect2Affect Isolation Assessment
Additionally, access to primary care providers (e.g. physicians, nurse practitioners) who routinely screen seniors for symptoms of loneliness is required to effectively treat loneliness in the senior population.
2. WHOLE-PERSON CARE MANAGEMENT
Seniors encounter numerous physical and emotional health challenges as they age. Diabetes, arthritis, hypertension, heart disease, and depression are all prevalent. Specifically, 80 percent of seniors have at least one chronic condition, while 68 percent have two or more often requiring specialized care. To complicate matters, financial insecurity is an issue for 70 percent of seniors, especially those on fixed incomes or government insurance programs (e.g. Medicaid and Medicare).
If left unattended, health costs for medications, hospital and physician services are at least 30 percent more for seniors who experience loneliness.
Treating loneliness requires a whole-person approach to care: physical, emotional, and financial. It extends beyond care provided by nurses and physicians to family members, caregivers, senior living facilities, and others. It includes pastoral care, financial counseling, home visits, and functional foods. As you read this, you may be thinking about the major investment these efforts would require. However, what would be the cost of doing nothing? If left unattended, health costs for medications, hospital and physician services are at least 30 percent more for seniors who experience loneliness.
3. TECHNOLOGIES THAT ENABLE MONITORING AND SELF CARE
The home environment for seniors is changing. Many live in multigenerational households or share a residence with others (e.g. assisted living, communal ownership, etc.). However, the majority lack longterm care insurance. Access to nursing homes, skilled nursing, and long-term rehabilitation facilities is also increasingly problematic due to cost.
It should also be noted that many seniors prefer to live independently at home, or in a senior living community. To better facilitate connectivity with seniors in their preferred environments, technology can help monitor their physical and emotional well-being, which can allow seniors to play a more direct role in their care. Technology can also play a major role in mitigating the harmful and costly complications of senior loneliness. Smart devices such as digital pill dispensers, motion activated lighting, smart doorbells, security systems, and devices that sense troubling symptoms will become standard for seniors. Such in-home technologies can strengthen connectivity, as well as reduce loneliness-induced anxiety and depression. Examples include:
- Let’s Be Authentic: Philadelphia-based video-chat app
- Quarantine Buddy App: platform where total strangers feeling anxious or lonely because of the pandemic can have virtual hangout sessions
- Paro: electronic harp seal developed for the memory impaired that reacts to touch, and can chirp, play games, as well as dance with seniors
- ChihiraAico: technology designed to resemble a 32-year-old woman and encourages the elderly to talk about their problems
- Pepper: technology that can read and respond to human emotions
- Encore Smart: assisted walker that can take seniors across even rugged landscapes
- Robear: robotic nurse that can carry a patient weighing up to 176 pounds
- Lively: technology that enables the placement of sensors on things like pillows, the bathroom door, key chains and medication boxes
4. REASSURING HEALTHCARE FACILITIES
Seniors use a wide spectrum of facilities and services often centered around hospitals and medical practitioners. However, most are constructed to optimize efficiency for caregivers. Patient experiences are typically a secondary concern.
Facility design matters. For lonely seniors, physical facilities that are inaccessible or uninviting lead to certain issues. Examples include misleading biometrics, inaccurate medical history reporting, missed appointments, nonadherence issues, and avoidable complications. Atmospherics, including lighting, colors and signage, also matter. They can instill a sense of wellbeing and confidence, as well as help mitigate loneliness among seniors requiring medical attention. Location also matters. Seniors prefer services close to home.
Senior living communities present a unique challenge for treating senior loneliness. Most operators assist their residents in accessing local medical facilities and offer select services on site (e.g. nursing care, pharmacy, nutrition, etc.). They also offer personalized therapeutic programs for loneliness and depression, plus have higher staffing levels. However, three out of five seniors cannot afford to live in private senior living communities. This emphasizes the need to reassure seniors within the healthcare environment, as they may not be able to receive needed care in their own homes.
ERDMAN Takeaway
Loneliness among seniors is prevalent, growing, and costly. A purposeful approach is needed to diagnose and treat senior loneliness. It should include screening, whole-person care, technologies that support connectivity, and accessible facilities that optimize patient experiences.
For more information about how your organization can create a dedicated program targeting loneliness in seniors, contact ERDMAN today. Our decades of experience designing for the care of others has offered countless insights and solutions that can help advance your care delivery models.
For more information, please contact us.

- Loneliness and the Workplace Cigna 2020 https://www.cigna.com/about-us/newsroom/studies-and-reports/combatting-loneliness/
- SocialPro. Report: Loneliness and Anxiety During Lockdown. (2020, April). Retrieved from https://socialpronow.com/loneliness-corona/
- Abbott, C. (2020, January 6). Senior living trends: Prepare for historic changes in 2020. Retrieved from https://www.mcknightsseniorliving.com/home/columns/guest-columns/senior-living-trends-prepare-for-historic-changes-in-2020/
- Jamie Ducharme “A Plague of Loneliness” Time June 22-29, 2020
- Murphy, S. L., Xu, J., Kochanek, K., & Arias, E. (2018, November). Mortality in the United States, 2017. Report No. 328. Retrieved from https://www.cdc.gov/nchs/data/databriefs/db328-h.pdf
- Woolf, S. H., & Schoomaker, H. (2019). Life Expectancy and Mortality Rates in the United States, 1959-2017. Jama, 322(20), 1996. doi:10.1001/jama.2019.16932
- Case, A., & Deaton, A. (2017). Mortality and Morbidity in the 21st Century. Brookings Papers on Economic Activity, 2017(1), 397-476. doi:10.1353/eca.2017.0005
- Stein, E. M., Gennuso, K. P., Ugboaja, D. C., & Remington, P. L. (2017). The Epidemic of Despair Among White Americans: Trends in the Leading Causes of Premature Death, 1999–2015. American Journal of Public Health, 107(10), 1541-1547. doi:10.2105/ajph.2017.303941
- Chen, Y., & Vanderweele, T. J. (2018). Associations of Religious Upbringing With Subsequent Health and Well-Being From Adolescence to Young Adulthood: An Outcome-Wide Analysis. American Journal of Epidemiology, 187(11), 2355-2364. doi:10.1093/aje/kwy142
- Cuijpers, P., Karyotaki, E., Eckshtain, D., Ng, M. Y., Corteselli, K. A., Noma, H., . . . Weisz, J. R. (2020). Psychotherapy for Depression Across Different Age Groups: A Systematic Review and Meta-analysis. JAMA Psychiatry, 77(7), 694. doi:10.1001/jamapsychiatry.2020.0164
- Holt-Lunstad, J., Smith, T. B., Baker, M., Harris, T., & Stephenson, D. (2015). Loneliness and Social Isolation as Risk Factors for Mortality. Perspectives on Psychological Science, 10(2), 227-237. doi:10.1177/1745691614568352
- United States Census Bureau. (2020, June 25). 65 and Older Population Grows Rapidly as Baby Boomers Age [Press release]. https://www.census.gov/newsroom/press-releases/2020/65-older-population-grows.html
- Senior Citizen Facts and Statistics 2020. (2020, July 28). Retrieved from https://www.suddenlysenior.com/senior-facts-and-figures/
- Coughlin, J. F. (2018, December 07). The Longevity Economy: Why Seniors Are a Fast-Growing Emerging Market. Retrieved from https://www.barrons.com/articles/seniors-have-spending-power-especially-as-life-spans-lengthen-1544226021



